The Battle to Reclaim Medicare
By Diane Archer
Big health insurers are chomping at the bit for Medicare business. They earn tens of billions of dollars in annual profits through the Medicare Advantage program. But, these insurers still claim they would cut benefits and raise costs for Medicare Advantage enrollees if the government doesn’t significantly increase their already inflated payments.
Since its inception, Medicare Advantage — an alternative to traditional Medicare in which private health insurance companies cover Medicare benefits — has cost the Medicare program more per enrollee than traditional Medicare, which is government-administered. Several independent experts say that Medicare Advantage now costs at least $88 billion more than traditional Medicare would cost for the same enrollees, eroding the Medicare trust fund and weakening the Medicare program.
Medicare Advantage enrollees do not benefit in meaningful ways from ever higher Medicare Advantage rates. The evidence suggests that insurers in Medicare Advantage too often wrongly deny enrollees critical care; they impose obstacles to care that don’t exist for people in traditional Medicare, including burdensome prior authorization requirements and restricted physician and hospital networks. Many insurance companies also regularly claim that their enrollees are sicker than they actually are to gain extra funding from the U.S. government — overpayments that have cost the government hundreds of billions of dollars. Out-of-pocket costs for complex care pose an additional barrier to care for Medicare Advantage enrollees.
In response, the Biden administration has implemented new rules to reduce wrongful delays and denials of care under Medicare Advantage. New polling from Data for Progress finds that these rules are popular with voters across party lines, including requiring Medicare Advantage plans to state the specific reason for denying prior authorization requests (76%), creating an online database for health providers to determine when a prior authorization is needed (74%), and cutting prior authorization decision times in half for some patients (72%).
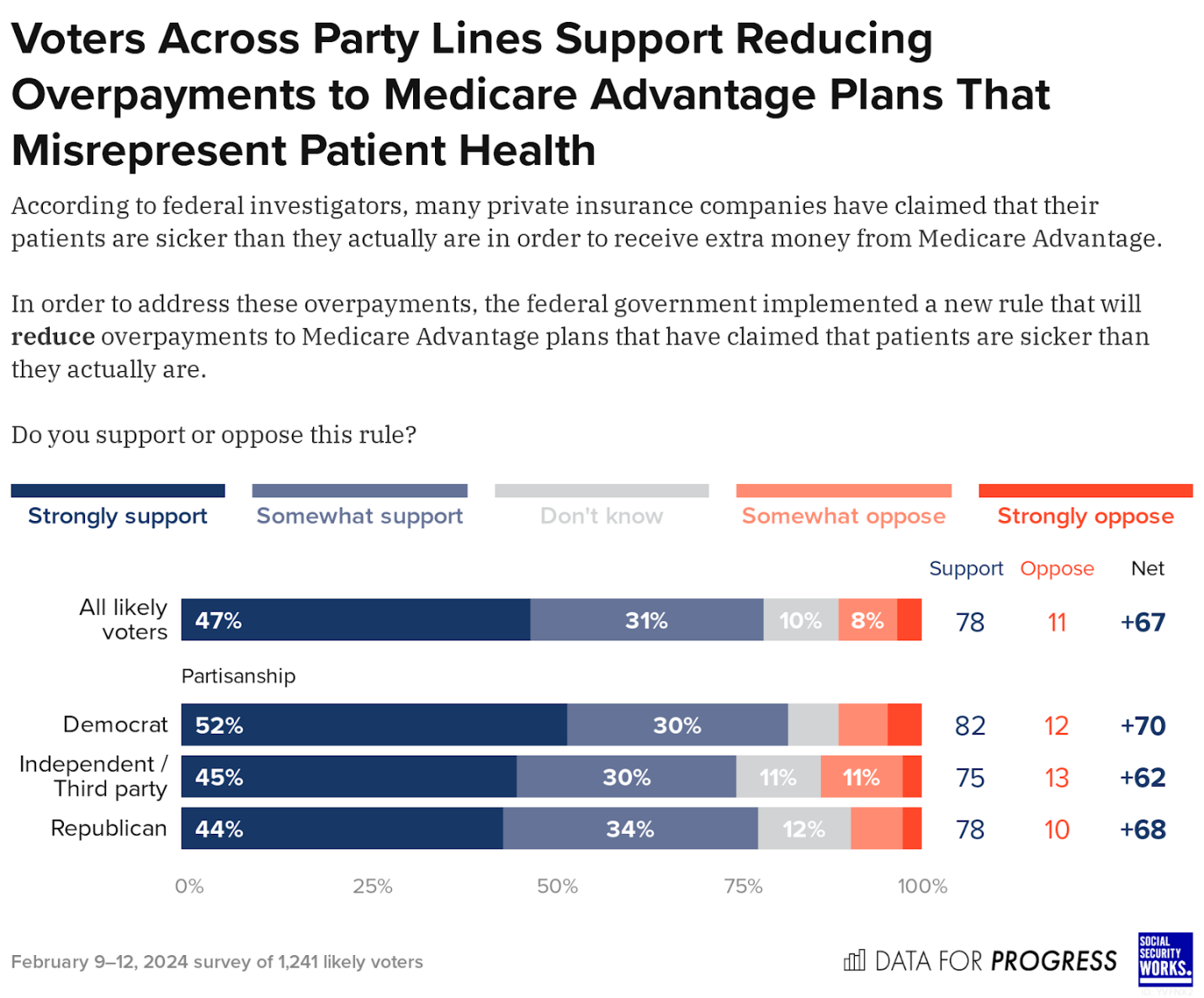
Voters across party lines also favor reducing overpayments to insurers offering Medicare Advantage plans. Nearly 4 in 5 likely voters (78 percent) support the Biden administration’s plan to keep insurers from overcharging the Medicare program. They don’t want the government to allow insurers to get higher payments because they claim their enrollees are sicker than they actually are.
These are important steps, but we need to go further. Our government still lacks the resources and the power to prevent insurers from inappropriate delays and denials of care and inadequate provider networks. It can’t ensure Medicare Advantage enrollees receive the benefits to which they are entitled.
One way that the Biden administration can go further is by ensuring that Medicare Advantage enrollees don’t have to pay out of pocket for care that is out of their network. Seventy-seven percent of voters support requiring Medicare Advantage plans to cover services from any medical provider that accepts Medicare’s approved rate.
What’s more, voters across party lines want the government to collect the hundreds of billions in overpayments from insurers. Around two-thirds of likely voters (67 percent) support aggressive collection of the funds that were overcharged.
Our government could also end the hundreds of billions in Medicare Advantage overpayments and use that money to strengthen traditional Medicare. Seventy-five percent of likely voters support this investment in traditional Medicare. It’s not only the politically expedient thing to do; it’s the right thing to do.
When traditional Medicare was enacted in 1965, it was with the promise of guaranteeing older adults easy access to the care they need, without an insurer middleman profiting by coming between them and their treating physicians.
When Medicare Advantage became law in 2003, there were no guarantees. Our government is spending more and enrollees are too often getting fewer Medicare benefits than they would in traditional Medicare.
The Biden administration must take further, stronger action to crack down on Medicare Advantage overpayments and wrongful delays and denials — much-needed policies that will help millions of Americans access and afford care, and are supported by voters across party lines.
Diane Archer is the president of Just Care USA, a digital hub that provides health and financial information for older adults and their caregivers. She serves as Senior Advisor on Medicare at Social Security Works. She is founder and past president of the Medicare Rights Center. From 2005-10, she led the Institute for America’s Future Health Care for All Project as its special counsel and project director during health care reform.